IMA BH Curriculum
Goals
- Improve familiarity with mental health within medicine
- Improve communication skills
Learning Objectives
- Use the Patient-Centered Interview (PCI) technique to gather psychiatric history with relevant subtleties based on patient, family, and system needs (Patient Care)
- Use the Ask-Respond-Teach (ART) framework to educate patients about diagnoses for unipolar mood and anxiety disorders (Interpersonal and Communication Skills)
- Understand the mechanisms, indications, and evidence for therapies for unipolar mood and anxiety disorders (Medical Knowledge)
- Use principles of measurement-based care (i.e. use of Patient Health Questionnaire-9 and Generalized Anxiety Disorder-7 (PHQ-9 and GAD-7)) to monitor and revise treatment (Patient Care)
- Coordinate patient care with available mental health resources including collaborative care psychiatry and community resources (Systems-Based Practice)
- Practice principles of Trauma-Informed Care (TIC) in order to establish and sustain therapeutic relationships with patients (Professionalism)
Sessions
Sextile 1. Orientation: slides refresher on MI
Sextile 2. Medication Management: 10min Pre-Video & slides
Sextile 3. Psychoeducation: slides
Sextile 4. DDx: preceptor guide
Sextile 5. Navigating the System:
Sextile 6. Final Didactic: slides or PGY-1
Expectations for Communication
- Determine patient’s understanding of symptoms or its cause. (For a patient with an already established diagnosis, this will apply for active symptoms and what the patient's perspective is of those symptoms, not simply the symptoms themselves. For a patient in remission this will simply be eliciting the patient's perspective that symptoms have remitted.)
- Reflect what patient is saying; show empathy and concern.
- Explain diagnosis, incorporating patient's informational needs. Connect language of symptom description to diagnosis. (For a patient with an established diagnosis, this could mean connecting which active symptoms fit that working diagnosis and/or how it will improve with treatment, e.g. "You mentioned worry is causing several problems like making it difficult for you to sleep and relax. This medication will improve worry." For a patient in remission, this will mean sharing our impression that the working diagnosis has remitted and why.)
- Discuss treatment alternatives.
- Explore patient preference on treatment choice.
- Use teach back.
Workflow for PGY-2's
1) Patient-Centered Interview Script
1) Introduce the patient to IMA BH
Welcome to our behavioral health clinic. My name is Dr. Sundaresh. I am a second year Internal Medicine resident who rotates in this clinic.
2) Set the agenda
Since this is your first time in our behavioral health clinic, I’d like to give you an idea of what to expect today. First I’d like to hear from you about your experience and how you think we can help. Some folks are looking for help finding a therapist. Others are interested in a medication. Some are not sure, and that’s ok too. Afterwards I will step out to review what we talked about with my attending before we finalize our plan.
3) Open-ended HPI
What brings you to our behavioral health clinic? [Listen]
4) Elaborate the HPI but keep it patient-centered
When did you first realize you were feeling that way?
5) Transition to the doctor-centered HPI
Thank you for sharing your experience with me.
I want to make sure I’ve understood everything correctly. I’m going to summarize what I’ve heard so far. Afterwards please feel free to make corrections or additions.
In order to get more information that will be helpful, is it ok if I go through a list of questions?
Responses for volunteered disclosures of trauma
“Thank you for telling me.”
“Thank you for sharing that with me.”
“I’m sorry that happened to you.”
2) Visit info (Rooming tab): Scheduled/Established: IMA Eval (free text)
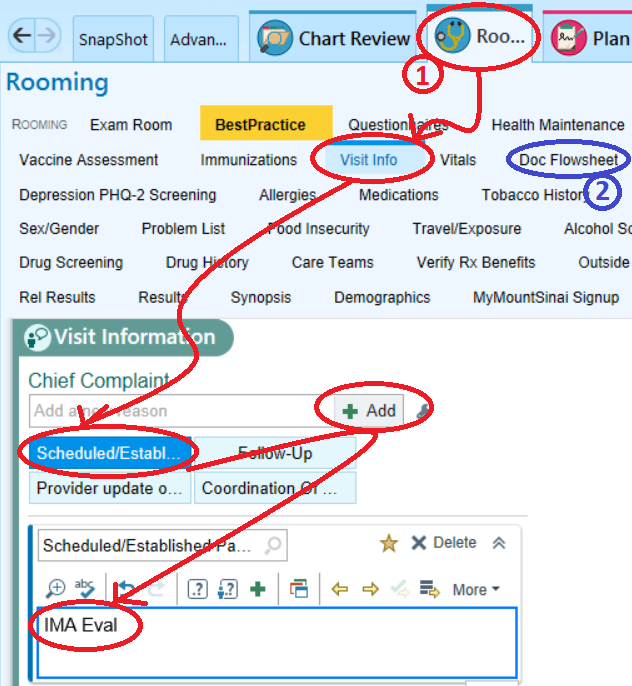
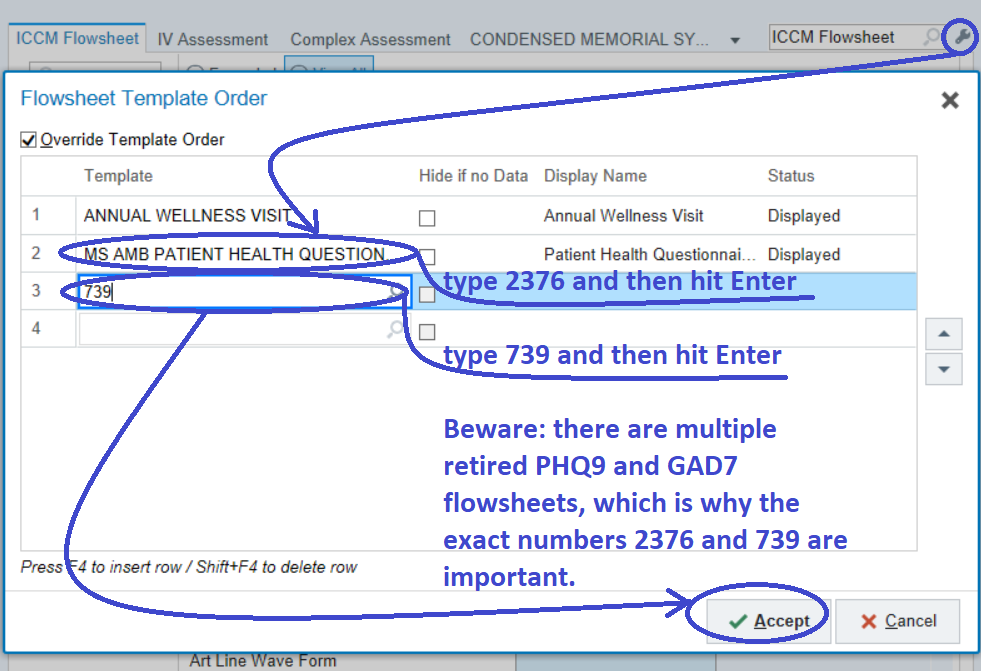
3) Doc flowsheet (Rooming tab): PHQ2/9 (2376) and GAD7 (739). Use these exact numbers. Patients who are seen in the office are handed a physical copy of these forms. Please transfer these manually into the flowsheet. For video visits you will need to ask the questions yourself.
4) Note: .EVAL
5) AVS: simply free-text guidance for medications, referrals, and follow up plan
Video visits: must be done with video either with Haiku or Doximity video dialer. We are no longer allowed to do audio-only visits.
Search the Careteam App for a video visit tip sheet.
Goals of IMA BH Clinic
1) Empathetically communicate and provide psychoeducation for a diagnosis.
DDx:
Mood disorders
Anxiety disorders
Trauma-related disorders
Personality disorders
ADHD
Substance use disorders
Neurocognitive disorders
Psychotic spectrum disorders
2) Medication management through IMA Eval visits.
3) Make referrals for behavioral interventions or psychiatry.
Depression Care Management (DCM)
1) Medicaid and Medicare with a PHQ9 or GAD7 score of at least 10 are eligible. Patients with commercial insurance are not eligible.
2) This is a short-term intervention where the patient receives brief weekly phone calls for 2-3 months.
3) Refer through AMB REF TO IMA BEHAVIORAL HEALTH
4) Epic chat IMA Depression Care Management for a warm handoff, if desired.
Psychotherapy
.IMABEHAVIORALHEALTHCOMMUNITYRESOURCE for patients with Medicaid or Medicare
.IMABHTHERAPYFINDERS for patients with commercial insurance
Psychiatry
1) Short-term IMA psychiatrist Daniel Suter for 1-4 consultative visits, via AMB REF TO IMA BEHAVIORAL HEALTH
2) Long-term psychiatry, via AMB REF TO IMA BEHAVIORAL HEALTH or dotphrases above.
3) Please contact Dr. Eric Woods with any patient questions via email or staff message.
4) Suicide screening and safety planning.
.SUICIDEIMASCREEN
.SAFETYPLANIMAENGLISH or .SAFETYPLANIMASPANISH (Steal from Shyam Sundaresh)
Mental Health Resources for IM Residents
Student & Trainee Mental Health Program (STMH)
FREE. Consultations, therapy, medications, referrals, burn out
212-659-8805
STMH@mssm.edu
Mental Health Hotline
24/7 crisis support, or information about referrals
212-241-2400, school code ICAHN
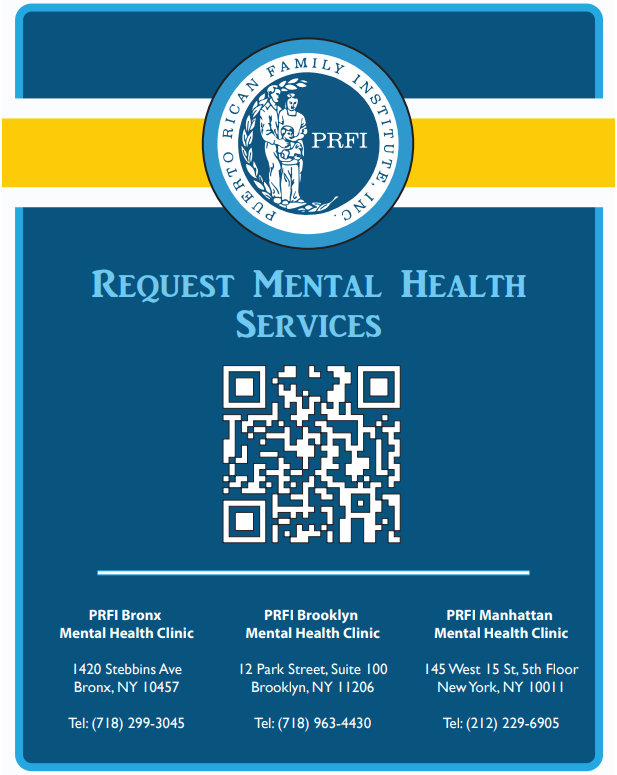
Puerto Rican Family Institute
Currently accepting patients with Medicaid WITHOUT Medicare for psychotherapy. They also have psychiatry.
Refer by completing this form.
Or have your patient complete this:
IMA Psychiatrist
Current consultative appts with the IMA psychiatrist are on hold. However please enter consult for “IMA BEHAVIORAL HEALTH” in EPIC and include specific referral question for psychiatry and the team will help connect the patient with ambulatory psychiatry if indicated. Referrals will be reviewed and plan communicated back to PCP via telephone message in EPIC within 2 weeks.
In the future the Ima psychiatrist will see patients at IMA for 1-4 consultative visits only. After these 1-4 visits, patients will either be referred back to PCP to continue medication regimen or referred to outside psychiatrist with the help of Triage SW.
Reasons for referral to psychiatry include: assistance with making psychiatric diagnosis, assistance with medication management for refractory depression/anxiety and other stable mental illness (e.g. bipolar disorder, schizophrenia). For all other referral reasons including controlled substance prescriptions, surgical clearance, paperwork completion, patient needing or interested in long-term care with a psychiatrist, or patient wishing to switch from their current psychiatrist, please refer to Triage SW (instead of referring to IMA Behavioral Health) for help in finding the patient an outside psychiatric provider.
Please contact Dr. Eric Woods with any patient questions via email or staff message.
Depression Care Management (DCM)
Eligibility is PHQ-9 or GAD-7 of >= 10, and Medicare or Medicaid. This is a behavioral activation protocol that happens over the phone for 10-20 minutes per week for 2-4 months. Refer with the IMA Behavioral Health referral.
Epic chat IMA Depression Care Management for a warm handoff.
IMA Psychiatrists
TBD
Program Director
EMPLOYEES Only: Mount Sinai CSRPG-Center for Stress Resilience and Personal Growth
CSRPG provides mental health treatment for Mount Sinai employees.
Employees (patients) should call or email to set up an initial evaluation or providers can reach out with permission from the patient.
Tel: 212-659-5564 (9am-9pm M-F)
Email: MS-CSRPG@mountsinai.org
Alternative Mental Health Options
To explore alternative referral options for this patient one may:
call or visit 1888-NYC-well (1-888-692-9355) NYCwell.cityofnewyork.us/en
visit www.hitesite.org or psychologytoday.org
Institute for Family Health, Center for Counseling and Family Health Center of Harlem 1824 Madison Avenue 2nd Floor New York, NY 10035 (Ph.) 212-423-4200 , (Fax) 646-770-8401 Center for Counseling of Harlem hours: Monday- Friday: 8:30am-8pm Saturday-Sunday: 9am-5pm Walk-Ins receive same or next day appointment
MSH Outpatient Adult Psychiatric Clinic Diagnostic Evaluations, Medication Management, Individual and Group Psychotherapy; Clozapine Clinic 20 East 106th Street, 9th Floor Or 1160 5th Ave New York, NY (bet. 5th and Madison Ave) http://www.mountsinai.org/patient?care/serviceareas/ psychiatry/areas?of?care/ambulatory?psychiatry?services General information, intake, and referrals: (212) 241- 5947, Julia Siegel Julia.siegel@mountsinai.org
MSH Partial Hospital Program Short term (2-6 weeks) intensive treatment (4-5 days per week) to prevent psychiatric hospitalization or to step down from psychiatric hospitalization 20 East 106th Street, 9th Floor New York, NY (bet. 5th and Madison Ave) http://www.mountsinai.org/patient?care/serviceareas/ psychiatry/areas?of?care/partial?hospital?program For Referrals Contact: Brittany Masi MHC Phone: 212 241-3170 Fax: 212-426-5107 Email: phpreferrals@mountsinai.org
Mount Sinai St. Luke's Outpatient Adult Psychiatry Diagnostic Evaluations, Medication Management, Individual and Group Psychotherapy; Clozapine Clinic; First Onset Psychosis services 411 West 114th Street, 3rd & 5th Floor New York, NY (off Amsterdam Ave.) http://www.stlukeshospitalnyc.org/Adult_Mental_Health.aspx If you are seeking services for yourself, a friend, or family member, please contact the Access Center at (212) 523-8080. If you are a mental health provider from the Mount Sinai Health System, please call (212) 523-5384
The Center for Intensive Treatment of Personality Disorders (CITPD) Short term DBT-based intensive group therapy 1000 10th Avenue, 6th Floor New York, NY (bet. 58th & 59th St) http://www.roosevelthospitalnyc.org/Services/Psychiatry/CITPD/ To arrange for treatment at CITPD, patients, families and providers can call the Comprehensive Assessment Center at 212-523-8080 to schedule an evaluation.
Union Settlement 2089 3rd Ave (at 114th St) NY, NY 10029 212-828-6144 (Intake Coordinator)
Upper Manhattan Mental Health Center 212-694-9200 Located on Amsterdam between 145th and 146th For substance use must request Chemical Dependence Program
Metropolitan Hospital 1900 2nd Ave 1st Floor New York, NY 10029 212-423-6645 Mon-Fri: Clients seeking individual treatment who are not being referred by an inpatient unit or clinician must walk-in for their initial appointment and arrive by 7:45 am
Student Trainee Mental Health - for Sinai students (medical and graduate), residents and fellows only. Takes most insurances. Call 212-659-8805 for an intake or email stmh@mssm.edu
IMA SW Triage: assistance in identifying resources and making appointments for mental health and substance use. Please place “Consult to Social Work” (NOT “Consult to IMA Social Work)
Alternative Substance Use Disorder Options
IMA REACH Program Email: # REACH
IMA SW Triage: Please refer to IMA Triage social worker for assistance in identifying resources and making appointments for mental health and substance use. Please place “Consult to Social Work” (NOT “Consult to IMA Social Work).
Mount Sinai West Addiction Institute of NY. 429 West 58th Street NY NY 10019, Contact: Mr. Stephen Torre. 212-523-8009.(Alcohol, Tx: Methadone/Suboxone, Stimulants, Sedatives, Cannabis)
Mount Sinai Beth Israel OTP. 429 2nd Avenue, NY, NY 10010, Contact: Georgina Spence-Hardy: 212-726-6800 (Opioid Tx: Methadone/Suboxone, Alcohol and benzodiazepine treatment)
Lower Eastside Service Center, Inc. (LESC) Outreach Coordinator: Dennis Murphy @ 917-217-3771 Opioid Treatment Program (outpatient): Contact: Jaime Holder@ cell 347-723-0859 or @ office 212-343-3584 46 East Broadway, NY, NY 10002 and 62 East Broadway, NY, NY 10002, Outpatient Treatment: Contact: Theresa Pension @ 212-343-3522 46 East Broadway, NY, NY 10002, Residential Treatment:Contact: Sabrina Mangual @ office 212-566-7590 or cell 347-538-2632 7 Gouvernuer Slip East, NY, NY 10002;
Smartphrase for alternative options:
.IMABEHAVIORALHEALTHCOMMUNITYRESOURCE